Sciatica
What is Sciatica?
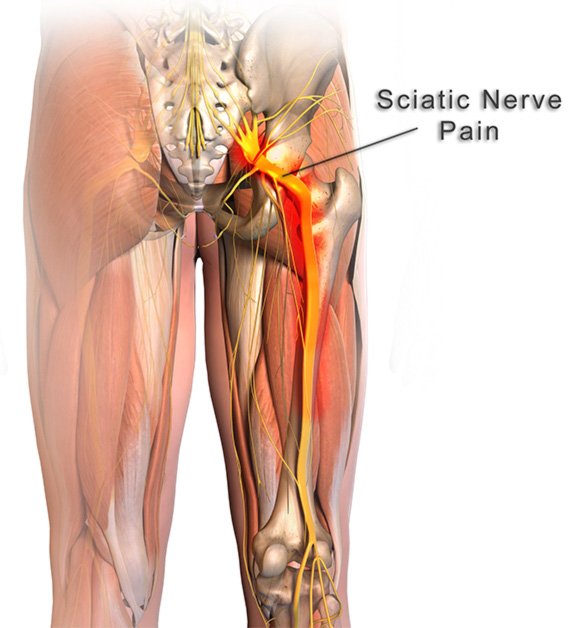
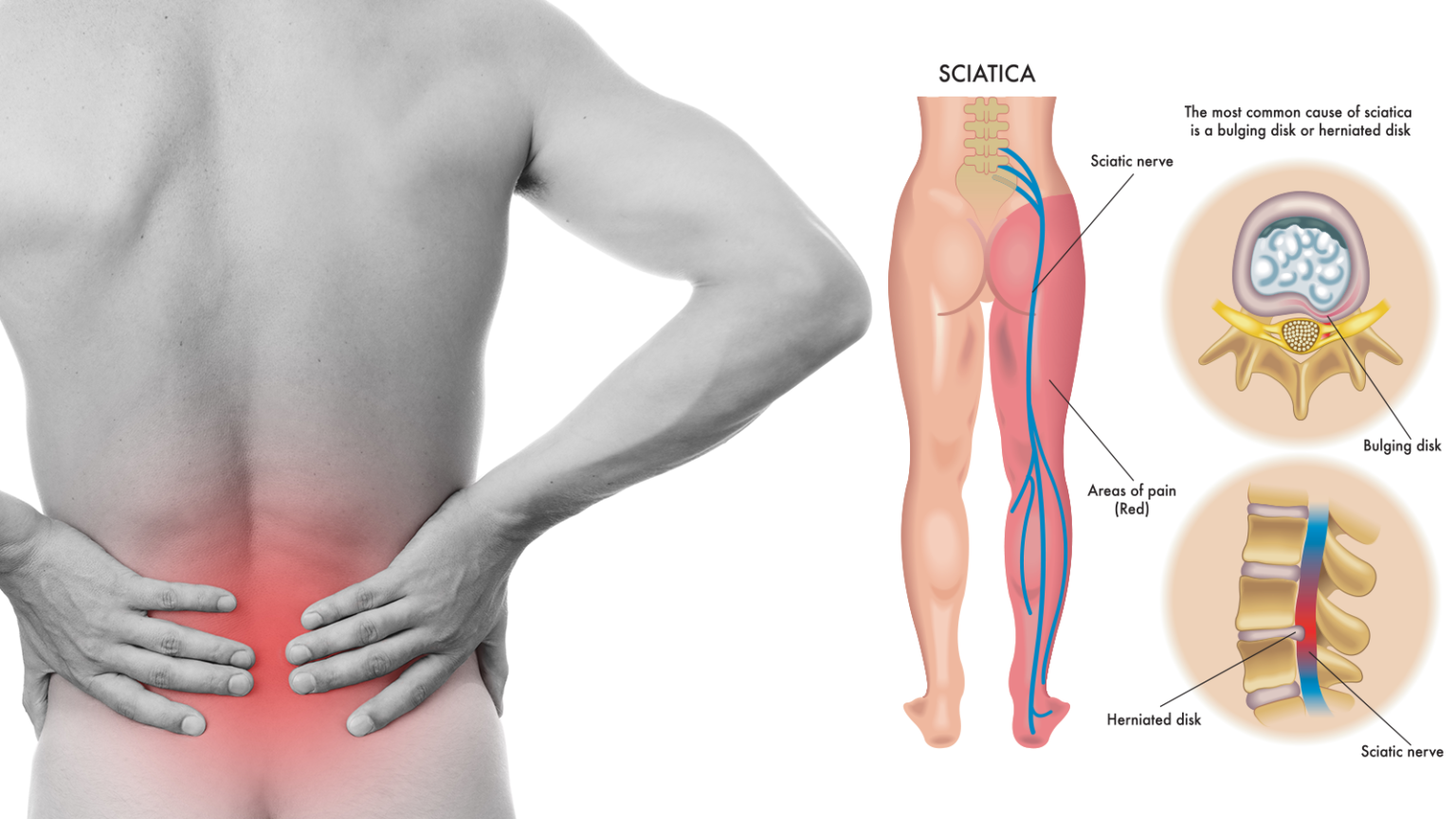
Sciatica refers to pain that travels along the path of the sciatic nerve. The sciatic nerve travels from the lower back through the hips and buttocks and down each leg. The symptom itself is really radiculopathy (or radicular pain), but because it is so common, and relates to a specific nerve, it is commonly referred to as sciatica.
Symptoms
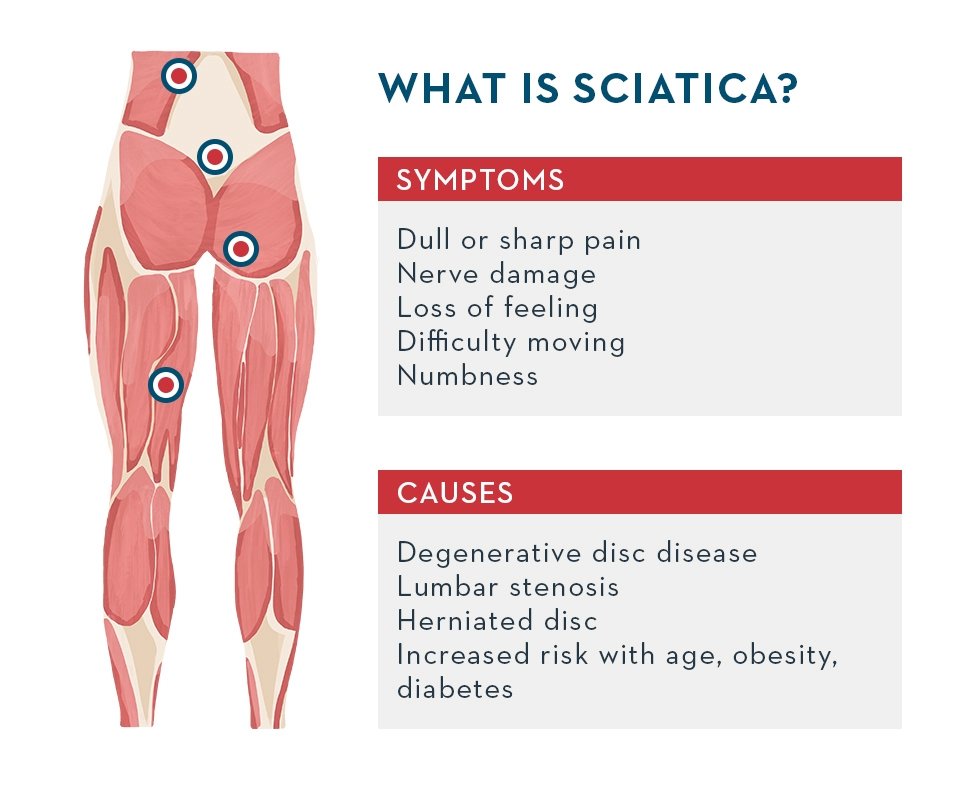
Symptoms associated with sciatica can range widely, typically dependent upon cause, but here are some of the most common:
Pain that travels down the buttocks or into the calf
Pain that is dull or sharp that radiates from the low back into the buttocks or below
Burning or tingling sensation in the buttock or down the leg
Loss of feeling in the leg
Difficulty moving the leg or walking
Weakness in the leg
Causes
Since sciatica is a symptom of an underlying condition most commonly associated with the following:
Bone spur
Obesity
Age-related conditions
Diagnosis
The most common imaging for this condition is MRI. X-rays of the affected region are often added to complete the evaluation of the vertebra. Please note, however, that some conditions that cause sciatica cannot be seen on plain x-rays. CT scan and myelogram were more commonly used before MRI, but now are infrequently ordered as the initial diagnostic imaging, unless special circumstances exist that warrant their use. An electromyogram is infrequently used.
X-ray: Application of radiation to produce a film or picture of a part of the body can show the structure of the vertebrae and the outline of the joints. X-rays of the spine are obtained to search for other potential causes of pain, i.e. tumors, infections, fractures, etc.
Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays; can show the shape and size of the spinal canal, its contents and the structures around it.
Magnetic resonance imaging (MRI): A diagnostic test that produces 3D images of body structures using powerful magnets and computer technology; can show the spinal cord, nerve roots and surrounding areas as well as enlargement, degeneration and tumors.
Myelogram: An X-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces; can show pressure on the spinal cord or nerves due to herniated discs, bone spurs or tumors.
Electromyogram and Nerve Conduction Studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury or whether there is another site of nerve compression. This test is infrequently ordered.
Treatment
Non-Surgical Treatments
The initial treatment for sciatica is usually conservative and nonsurgical in the form of rest, medications (including oral steroids), physical therapy, bracing, and injective therapy.
Sciatica is most commonly treated with both steroid-based and non-steroid anti-inflammatory medication, if the pain is only mild to moderate. Our spine specialists may also recommend a course of physical therapy. Our physical therapy team will perform an in-depth evaluation, which, combined with the doctor's diagnosis, dictates a treatment specifically designed for patients with sciatica. Therapy may include pelvic traction, gentle massage, ice and heat therapy, ultrasound, electrical muscle stimulation and stretching exercises. Pain medication and muscle relaxants may also be beneficial in conjunction with physical therapy.
An epidural steroid injection may be performed utilizing a spinal needle under X-ray guidance (through the use of a c-arm) to direct the medication to the exact level of the disc herniation for more moderate to severe symptoms.
Surgery
A doctor may recommend surgery if conservative treatment options, such as physical therapy and medications, do not reduce or end the pain altogether. Doctors discuss surgical options with patients to determine the proper procedure. As with any surgery, a patient's age, overall health and other issues are taken into consideration.
The benefits of surgery should be weighed carefully against its risks. Although a large percentage of patients with herniated discs report significant pain relief after surgery, there is no guarantee that surgery will help.
A patient may be considered a candidate for spinal surgery if:
Radicular pain limits normal activity or impairs quality of life
Progressive neurological deficits develop, such as leg weakness and/or numbness
Loss of normal bowel and bladder functions
Medication and physical therapy are ineffective
The patient is in reasonably good health
Lumbar laminectomy, also called open decompression, is a surgical procedure performed to treat the symptoms of central spinal stenosis or narrowing of the spinal canal. The surgery involves removal of all or part of the lamina (posterior part of the vertebra) to provide more space for the compressed spinal cord and/or nerve roots.
Lumbar discectomy is a type of surgery to fix a disc in the lower back. This surgery uses smaller cuts (incisions) than an open lumbar discectomy. During a minimally invasive lumbar discectomy, an orthopedic surgeon takes out part of the damaged disc. This helps ease the pressure on the spinal cord. Your surgeon can use different methods to do this. With one method, your surgeon inserts a small tube through the skin on your back, between the vertebrae and into the space with the herniated disc. He or she then inserts tiny tools through the tube to remove a part of the disc. Or a laser may be used to remove part of the disc. Unlike an open lumbar discectomy, the surgeon makes only a very small skin incision and does not remove any bone or muscle.
Lumbar interbody fusion is a surgical technique that attempts to eliminate instability in the back. A MAS® TLIF achieves this by using a less invasive approach to fuse one or more vertebrae together to reduce their motion. In a MAS® TLIF procedure, rather than starting from the middle of the back and spreading the muscles to the sides like in a traditional back surgery, the MAS® TLIF approach starts off to one side of the back and splits (rather than cuts) the back muscles in one direction. This allows the surgeon to make a smaller incision with less muscle injury, which may result in less postoperative pain and a quicker recovery. This approach has proven to reduce blood loss, minimize scarring, reduce length of hospital stay, and allow for patients to recover quicker than conventional lumbar fusions. At Aptiva Health, our orthopedic spine surgeons specialize in the MAS® TLIF procedure.